Victoria fights back COVID-19, but at what cost?

Mitchell Atanasovski pictured with his canine companion, Archie, said “my dog helped me through my darkest days.”
Mitchell Atanasovski, aged 23, was looking forward to finishing his double degree and travelling in 2020. COVID had other plans.
He found the first lockdown hard enough. A self-described extrovert, Mitchell thrives on being around other people and he felt extremely isolated.
His first major setback was when his graduation was cancelled. As the first person in his family to go to university, it was expected to be a proud moment for his mum.
Mitchell’s father passed away the year before he started university, so his graduation was supposed to be a special family occasion. It didn’t happen.
But it was during the second lockdown that Mitchell fell apart.
“I have never felt so low and broken in my entire life.”
Mitchell Atanasovski
His university studies had finished, he had no job and he couldn’t play sport or go to the gym.
“I went downhill. I struggled deeply with anxiety and stress. I had a feeling of extreme distress… and I crumbled. I couldn’t get out of bed, couldn’t eat, started vomiting and lost every inch of motivation and drive I’d ever had”, he said.
From June right through to August, Mitchell struggled with severe psychological distress that prevented him from doing anything at all.
“The things I miss are seeing my friends through playing sport, especially football. Missing out on this part of my life has had a big impact on my mental health.”
Mitchell crawled back out of his deep black hole by seeing a psychologist and setting himself a fitness goal. After months trapped inside his tortured mind, he decided to start running.
Running made him want to eat again and motivated him to get out of bed. It became a focus to occupy his mind and helped to banish dark thoughts.
Several weeks later, Mitchell began to feel better. He still has some dark days, but he is much better than before.
But things still don’t seem quite right.
“It feels weird when I catch up with friends now. We’re all worried about social distancing. It’s going to be hard socializing again…Everyone’s going to be stressed about spreading the virus and will be a bit paranoid about having close contact with each other.”
Impact of the Pandemic on University Students: Survey Results
Leading mental health experts are worried the pandemic has had a disproportionate effect on young adults. Youth mental health expert, Professor Pat McGorry has called it a “shadow pandemic” and says there is a “risk of scarring a whole generation.”
During the course of our investigation, we surveyed 100 tertiary students studying at three different universities in Melbourne. Social media platforms were used to distribute the anonymous survey to the students. Whilst it’s a small snapshot and not statistically representative, the results of our survey show that 90% of students have experienced a negative mental health impact from the pandemic lockdowns in Victoria.
When students were asked how they feel about lockdown, 76% said they felt angry, depressed, worried or anxious. A further 14% felt relieved that the lockdown was keeping them safe from the virus.

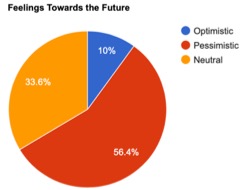
Our results also showed that almost 60% of students are pessimistic or stressed about the future, indicating that the pandemic may have long-lasting effects for many.

Click to listen to an audio recording of some anonymous student responses from our survey.
Flattening the Curve and Crushing COVID
Australia seemed to fare well in the beginning of the pandemic: as case numbers escalated worldwide, we seemed to avoid a catastrophe.
Success didn’t last long. The hotel quarantine debacle that unleashed Victoria’s second wave led to a longer, harder lockdown than the first, and several hundred deaths in aged care.
The novelty of the first lockdown was replaced with pandemic fatigue in the second. Gone was the enthusiasm for baking sourdough bread, reading books and hosting Saturday night drinks on zoom.
Extreme social isolation and loneliness set in.
“I feel like a prisoner in my own home”, was the way one survey respondent described it.
There is growing disquiet about the burden carried by young adults. The focus, understandably, has been on saving elderly and vulnerable lives to COVID, but what has this cost our youth?
Professor Pat McGorry predicts a long-lasting impact on young adults who he said “are facing a perfect storm which is undermining their mental health, threatening their futures and even their lives.
Mental ill health…is increasingly driven by potent risks arising from lockdown, the economic collapse due to COVID and the overhanging threat of climate change and escalating insecurity in their lives.”
Young Adults Seeking Treatment in Record Numbers
Doctor Julie Doswell, a GP at a large practice in Melbourne, said she has never seen a mental health crisis of such magnitude in over 30 years of general practice.
“Due to the extended harsh lockdown…the young adults I treat are in anguish, despair and have no hope…it is devastating seeing the effect lockdown has caused them. Access to psychiatrists and psychologists is now almost impossible.”
Psychologist Mr Tom Cartmill said that he and his colleagues had such a big surge in demand that the practice at which he works, Cova Psychology, had to knock back at least 15 new patients a week during the peak of the second lockdown.
Mr Cartmill expects there will be long-term mental health problems after the pandemic with things like “elevated anxiety, an increase in obsessive compulsive disorder presentations, increased dependence on digital media and a reduction in social skills.”
Extreme isolation pushed some young adults to extreme and dangerous behaviours.
“Some young people I treat are engaging in risky sexual behaviours…using different dating accounts to hook up for casual sex with random people…being starved of social contact is driving some people to do dangerous things”, Mr Cartmill said.
Clinical psychologist, Ms Linda Bennett, also said that young adults are suffering extreme distress. She predicts addiction will worsen in this demographic, with alcohol and drugs being used as self-medication to alleviate feelings of stress and social isolation.
Already, she has seen a big uptick in young people becoming addicted to drugs and alcohol. Her anecdotal evidence is borne out in data from the National Drug and Alcohol Research Centre.
Research from their Australians’ Drug Use Study shows that of those young adults who were occasionally using drugs and alcohol before the pandemic, there has been a 59% increase in cannabis use and a 42% increase in alcohol use since the beginning of restrictions.
“Many young adults are on JobKeeper, JobSeeker, or working from home. I’m seeing young people starting to use alcohol and marijuana daily, who had previously used these on a recreational basis only, just to cope with the loneliness,” said Ms Bennett.
Professor Andrea Reupert, Director of Psychological Programs at Krongold Clinic, said, it’s “the isolation and loss of physical interaction” that has caused the most damage.
“Autonomy and connectedness are the two most important elements to good mental health, and they were taken away from us. That is going to be very damaging in the long-term.”
Success crushing COVID has led to a different crisis
We’ve managed to prevent hospitals being overwhelmed by COVID-19 patients, but we now have a different crisis on our hands. Melbourne hospitals have been inundated with mental health patients who are sometimes waiting for days in emergency departments.
There has been an estimated 33% increase in young people presenting to emergency departments with self-harm injuries compared with last year. And mental health presentations are now outweighing all other medical presentations.
Ambulance Victoria’s Executive Director of Clinical Operations, Associate Professor Mick Stephenson said that of concern is the rise in calls to acutely mentally ill patients.
“What we have noticed in terms of the difference between the first and second lockdown in relation to mental health is that the acuities are higher this time around. We’re being called to more mental health patients, and of note they are sicker and their mental health symptoms are more severe”, he said.
A comprehensive Monash University study, led by Professor Caroline Gurvich, Deputy Director Monash Alfred Psychiatry research centre, was completed during the first lockdown in April and May. Over one-month, 1500 Australians were surveyed.
It found that 47% of respondents reported at least one post-traumatic stress disorder (PTSD) symptom, and suicidal thoughts were reported in 17% of females and 14% of males.
Professor Gurvich said, “The level of change, uncertainty and disruption to daily lives is substantial. We may see ongoing mental health problems including stress, anxiety, distress, depression, grief, loss and the emergence of PTSD symptoms.”
Indicating further signs of mental anguish is the sharp rise in eating disorders, with an explosion of young people requiring hospitalisation.
Belinda Caldwell, CEO at Eating Disorders Victoria, said “All major hospitals are reporting approximately a 50% increase in ED admissions to hospitals currently.”
“In young people we are seeing a significant increase in new onset eating disorders. The pandemic has created an environment for eating disorder behaviours to thrive…the uncertainty of the pandemic has brought about feelings of anxiety and loss of control…Social isolation and the loss of normal activities has also removed social layers that are important for recovery.”
“When the physical health pandemic ends I believe we’ll be moving into a mental health pandemic that will last longer than what we’ve seen with COVID.”
Mr John Brogdan, AM, Chair Lifeline
Melbournians seem jubilant about the easing of restrictions; eagerly making bookings at their favourite restaurants. But many young people are still dealing with significant mental wounds.
Second year undergraduate student, Maddi Casey, 19, has been hit hard by the pandemic.
“I guess it’s not just about what I’ve missed this year. It’s the worry and the uncertainty about how long the pandemic will impact on my plans for the future”, said Maddi.

“I lost my job in mid-March. I have applied for dozens of jobs and keep getting rejected… it has made me feel invalidated and destroyed my confidence.
The lack of routine and social isolation has affected me. There were days I’d get up at 2pm. I was going to bed at 5-6am when my dad was leaving for work. My world was upside down…
I used to be much more resilient……I feel helpless, fearful and defeated.
Once I realised that the pandemic was going to have a long-term impact on my mental health, I decided to get help from a psychologist. I have regular zoom sessions and they work really well…
I’m very anxious about returning to face-to-face learning in 2021 due to the health risks of COVID and it spreading again. It worries me a lot”, she said.
Telehealth has been a game changer in pandemic mental health support
Mental health experts agree that young people have been severely and disproportionately affected by the pandemic. But as part of a generation dubbed “digital natives”, technology is playing a role in reducing the impact on their mental health.
Reach Out Australia, an online mental health service for young people, has seen a “spike in click throughs to the ‘urgent help’ section of their website during the pandemic” indicating the extreme distress young people are experiencing.
Research Coordinator Ms Louisa Welland said that with limited access to mental health services during the pandemic, many young people have turned to Reach Out’s digital tools and online peer support forum to bridge that gap.
“Reach Out’s peer support forums have had a big increase in activity during the pandemic. These forums facilitate a community of young people who can post questions anonymously with the chats moderated by trained peer support volunteers.”, she said.
Other online services and helplines have cited increased traffic during the pandemic. In Victoria this year, Kids Helpline has experienced a 61% increase in calls, Beyond Blue a 67% increase and Lifeline a 40% increase.
A study published by Evaluation Journal of Australasia in conjunction with Beyond Blue found that online and telephone psychological support “reduced distress and increased ability to cope” and had “lasting positive effects” on mental health.
People can access a mental health practitioner more easily using digital tools and achieve better outcomes than using traditional therapy alone, said Mr Yianni Serpanos Founder and Director of digital health platforms HealthTechX and coreplus.
“Using digital tools to manage health has proven to be efficient, effective and produces a higher adherence rate than traditional health care delivery”, he said. Mental health clinicians can monitor progress, set goals and communicate with patients through apps such as NovoPsych.
Self-help apps like Perx Health allow patients to track their own progress and set reminders for medication and self-care routines.
Ms Caldwell said that at Eating Disorders Victoria “telehealth has broken down accessibility barriers… we have seen a 26% increase in contacts to our helpline…compared to the same 6 -month period last year. We’ve also been able to introduce new telehealth support options…some of our online support groups are now booked out till the end of the year.”
“Telehealth has enabled mental health clinicians to expand their services in a profession that does not have enough clinicians to meet demand during the pandemic. Probably the most important thing we’ve seen is the investment in telehealth”
Mr Angus Clelland CEO, Mental Health Victoria.
The pandemic has accelerated the use of telehealth and digital health care, providing accessibility to those who need urgent mental health care and throwing a lifeline to those who desperately need one.
The Australian Psychological Society said that more than 94% of psychologists have used telehealth during the pandemic and said that it “has quickly become a popular and effective modality for psychologists.”
While the APS welcomed the government’s announcement to double Medicare funded psychology sessions and extend telehealth, “we will continue to call on the government to secure the future of telehealth by making it permanently available for the delivery of psychological services.” Expanded telehealth and increased Medicare funded psychology sessions are set to end on March 31, 2021.
Telehealth has helped, but urgent reform is needed in a sector that was already under strain. According to Professor McGorry “Australia is better placed than most countries to respond because we have built a base camp of safe and trusted care spaces through the headspace platform.
But this base camp urgently needs to be built upon to guarantee multidisciplinary care for young people with complex needs and longer-term support. This, combined with affirmative action…and other reforms to safeguard the potential of our next generation, are urgent national priorities.”
If you or anyone you know needs support call Lifeline 13 11 14, Beyond Blue 1800 512 348, Kids Helpline 1800 55 1800, or Eating Disorders Victoria 1300 550 236.










